As a breastfeeding mother (of 3 kiddos), one of the biggest responsibilities is to ensure that our little ones are getting the best nutrition possible. However, when we suspect our child is sick from a food allergy, it can be a confusing and daunting experience. One way to figure out if your child is allergic to something you’re eating is through an elimination diet.
A food elimination diet for breastfeeding moms can be confusing, as you are actually removing the suspected allergens for your child, and not always for you too. This means removing certain foods from your diet for a set period of time to see if it improves your baby’s symptoms. If you suspect your baby has a food allergy, it’s important to consult with a healthcare provider to determine the best course of action for you and your child. In this blog post, I’ll share my experience and some tips on how to start a food elimination diet while breastfeeding.
Identifying the Problem
The first step to starting a food elimination diet for a breastfeeding mom is identifying the suspected problem food or foods, as we had in my case all 3 times. You may be wondering how to determine if your child has a food allergy. Food allergies can manifest in different ways, but the most common symptoms in babies include:
- Skin rash or hives
- Diarrhea or vomiting
- Colic or excessive crying
- Congestion or difficulty breathing
- Swelling of the face, lips, or tongue
- Fussiness during or after feedings
If you have read my other post on Identifying Tongue and Lip Tie in your Young Child, you may be thinking this list looks similar. And, thats the tricky part. It could be a food allergy + another feeding issue like oral ties. If your baby is exhibiting any of these symptoms, it’s important to speak with a healthcare provider who can help you determine if it’s a food allergy or another issue. Once you have a diagnosis, you can begin the process of eliminating potential allergens from your diet. You will note in my post about tongue and lip tie and in my course on Feeding Issues, that some of these symptoms overlap and are the same.
Starting an Elimination Diet
Starting an elimination diet can be overwhelming, but with the right preparation, it can be done successfully. Here are some tips to help you get started:
- Consult with a healthcare provider: Before starting an elimination diet, it’s important to consult with a healthcare provider who can guide you through the process and ensure that you and your baby are getting the necessary nutrients. I can not include this disclaimer enough. Trust your healthcare professionals and ask lots of questions. Remember, this is NOT always (and most often, not in my experience) your pediatrician. It could be your lactation consultant, your chiropractor, your immunologist or allergist, etc.
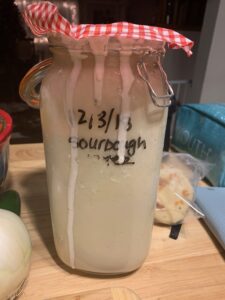
- Keep a food diary: Keeping a food diary can help you track what you eat and any symptoms your baby experiences. It can be helpful to write down what you eat, the time of day, and any symptoms your baby has after feeding. For us, this meant diaper checks. Did it ever. This was the first flag for us that something was wrong, on top of large spit ups, crying (colic) for long periods of time, and skin rashes.
- Start with the most common allergens, oftentimes called the top 8: The most common allergens that can be passed through breast milk are dairy, soy, wheat, egg, nuts (peanuts and tree nuts), fish, and shellfish. You can start by eliminating one food at a time for at least 2-4 weeks to see if there is any improvement in your baby’s symptoms. If there is no improvement, you can move on to the next potential allergen.
- Read labels carefully: It’s important to read labels carefully and understand the ingredients in the foods you’re eating. Many packaged foods contain hidden allergens, so it’s important to be diligent in your research. We found that this is particularly confusing with wheat, dairy and soy. There are so many hidden words for these things! We found that Free to Feed has the most helpful list of common used words and overall, general resources for breastfeeding with allergies so you should definitely check out all things Dr. Trill.
- Find substitutes: Eliminating certain foods from your diet can be challenging, but there are plenty of substitutes available. For example, if you’re eliminating dairy, you can substitute with plant-based milks like almond or coconut milk. I think this can be really hard and confusing, especially if you live in an area that doesn’t have a lot of options. I have found this particularly difficult for dairy-free and gluten-free, especially when traveling. Just because my local Walmart carries a lot of these alternatives, doesn’t mean that the Walmart in small-town Michigan where we are camping does. All stores are not created equal, and are stocked based on how their local shoppers purchase items.
- Stay hydrated: It’s important to stay hydrated during an elimination diet to ensure that you and your baby are getting enough fluids. Drinking plenty of water and herbal teas can help you stay hydrated.
- Seek support: Eliminating certain foods from your diet can be challenging, so it’s important to seek support from friends, family, or a support group. I talk about this a lot in my Managing Feeding Issues course. People are not always receptive to food allergies or supportive, and this can unfortunately include partners/spouses. Make sure you are educated on the facts so that you can talk to others about the details and help explain. I include family and support scripts in my course that help navigate this tricky area.
Reintroducing Foods
Once you have eliminated potential allergens from your diet and your baby’s symptoms have improved, it’s time to start reintroducing foods back into your diet. It’s important to reintroduce one food at a time and wait at least 3-4 days before introducing another food. This allows time for any potential allergic reactions to manifest. I know that my Allergy specialist felt strongly about not staying restricted if I didn’t have to, and she was anxious to get me eating the foods again that had proved not to be a trigger for us, i.e. eggs and nuts, which we had initially suspected.
If you notice any symptoms in your baby stop the reintroduction. For instance, my son is now two and we have had quite a bit of instances with 4 older siblings in the house where he has gotten into something he should not have – a biscuit left unattended on the table, a bite of brothers yogurt, etc. and we know immediately. He gets a rash around his mouth, eczema on his skin and bad bad bad diapers. We know that it is not time yet for reintroduction. I am still breastfeeding at night as well, and he still has reactions to my breastmilk if I accidentally eat something that I didn’t realize had dairy, was rice based and I missed it, etc.
And, it’s possible that it’s time to get an allergy test if you have not already gotten one. It is important to note that there are two different types of food allergies- so it’s important to understand what they are, what they mean, and how serious they are. The website, Everlywell, gives a very simple explanation of the definitions here:
Depending on the severity of the reaction, different immunoglobulins are used. The body’s three food-related immunoglobulins include [1]:
- Immunoglobulin E (IgE) – A rapid immune response that can be triggered by food
- Immunoglobulin G (IgG) – A more delayed and potentially more mild immune response that can be triggered by food
- Immunoglobulin A (IgA) – An antibody that can support the immune functions of mucous membranes
To summarize, the IgE is more serious and immediate – you are dealing with hives, trouble breathing, and anaphylactic reactions. Think – debilitating and even fatal. Like, you need to carry an epi-pen at all times and there is a high probability of needing hospitalization depending on the severity of ingestion and reaction. Luckily, none of my kids have this, but if you do, you can get through it. There are support systems and ways that you can work with your school, daycare, or elsewhere to make sure your kid is safe no matter who is with them.
IgG is a food sensitivity but as Dr. Trill says, is still a real food allergy and reaction. This includes stomach aches, cramps, and visible symptoms like the ones listed in the beginning of this article, i.e. diarrhea, mucus or blood in stool, skin rash, etc. but it tends to be more delayed – a few hours after eating, to even the next day, unliked IgE which is immediate. This is what my kids have, and let me tell you, just because its not anaphylactic, doesn’t mean it isn’t serious! My kids get all of these symptoms- I always know when they are exposed. My littlest especially gets a rash around his mouth, on his trunk and lower body, as well as horrible diarrhea that gives him skin burns. He is miserable for days at a time and it’s so sad to watch. It makes me have flashbacks to when he was a baby and I was desperately searching for the culprit and for support. Those were dark days and I don’t wish them upon anyone.
Was this helpful? Make sure to subscribe to our blog for more, and to check out our Managing Feeding Issues in Children course if you want more in-depth support!
If you like what you’re reading, make sure to subscribe to the blog!
Follow us on Instagram & Pinterest here for more content like this!